Neuroscience research is both professional and personal to James Lechleiter, Ph.D., professor of cellular and structural biology in the School of Medicine. “I’m interested in long-term degenerative diseases, as well as acute brain injuries, like stroke,” he says. “My wife, Patricia, has a neurodegenerative disease. We don’t know its underlying cause. My father died of a stroke and my grandfather was disabled by one when he was in his sixties, so brain diseases are part of my family. I’m always looking for things that could benefit or help heal the brain.”
At the end of 2013, Dr. Lechleiter received U.S. patent No. 8,618,074 for his discovery that a class of compounds is protective against traumatic brain injury (TBI). It was a watershed moment after seven years of diligent work, and yet this Minnesota native knows much more can be done in this area. He seeks to further the research to the point where development of potential therapies for TBI might be translated to practical application.
Imagine it: Any time a soldier is felled by an IED blast (improvised explosive device) or a high school football player goes down with a concussion, a pill could be administered to enhance healing and prevent years, even lifetimes, of headaches, behavioral changes and other damaging effects of the original injury.
An inside job
Dr. Lechleiter’s approach, in essence, encourages the brain to heal itself. “TBI is connected to long-term cognitive problems and deficits,” he says. “My studies look at stimulating natural processes to take care of the nervous system.”
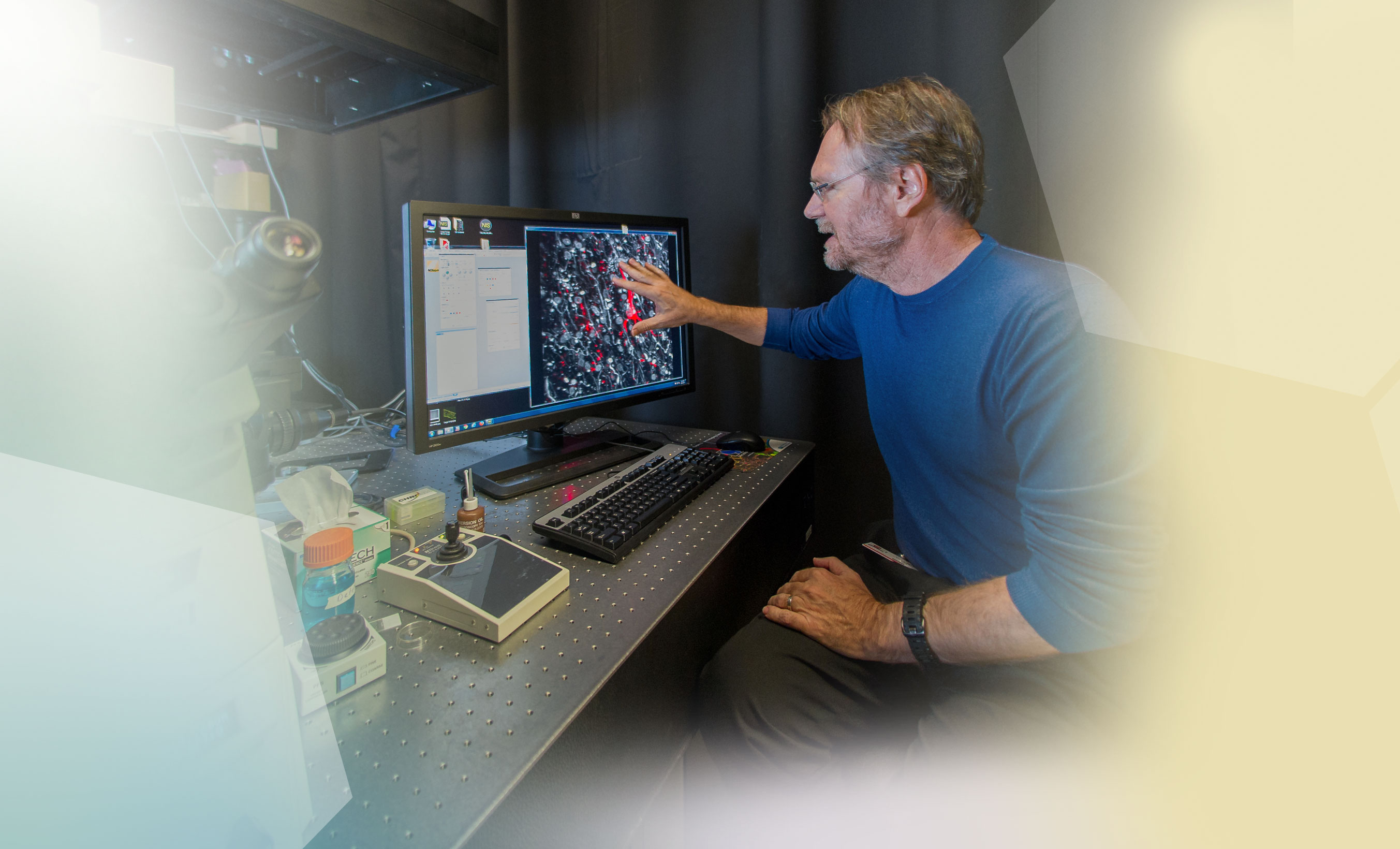
Two compounds stimulate the ability of astrocytes (caretaker cells) to do their job, Dr. Lechleiter found. These beneficial compounds are called purinergic receptor agonists, and one function is to control edema, the swelling that compresses brain tissue and neurons while increasing pressure inside the skull.
Dr. Lechleiter and colleagues have published studies showing that, in cells, brain tissue and live mice, treatment of the astrocytes with these compounds significantly reduced the edema. Importantly, more nerve cells — called neurons — survived. Most recently, the team found this to be true even in human brain tissue, which was obtained from patients who underwent surgery to treat epilepsy. Death of neurons is a common feature of degenerative diseases.
Time bombs
External signs and symptoms of TBI are not always present or can go unnoticed for prolonged periods. Currently, the treatment for patients is rest, and symptoms are only addressed when they are observed and the damage has become chronic.
“Undiagnosed traumatic brain injuries are time bombs,” Dr. Lechleiter says. “These injuries continue in the brain. They may have occurred on the battlefield, the ball field or the scene of a car accident, but then they are carried home.”
Once Dr. Lechleiter completes preclinical studies of this novel method of treating TBI, drugs that stimulate astrocytes will be entered into clinical trials to evaluate their therapeutic potential and safety in people.
“We’re very excited about the clinical impact of our findings and hope this success leads to new drug therapies for people with multiple types of brain injuries,” Dr. Lechleiter says.
There may be shared mechanisms between TBI and degenerative diseases such as Alzheimer’s and Parkinson’s, he says, which provides him hope on a personal level:
“I imagine at some point it could be beneficial to my wife, too.”